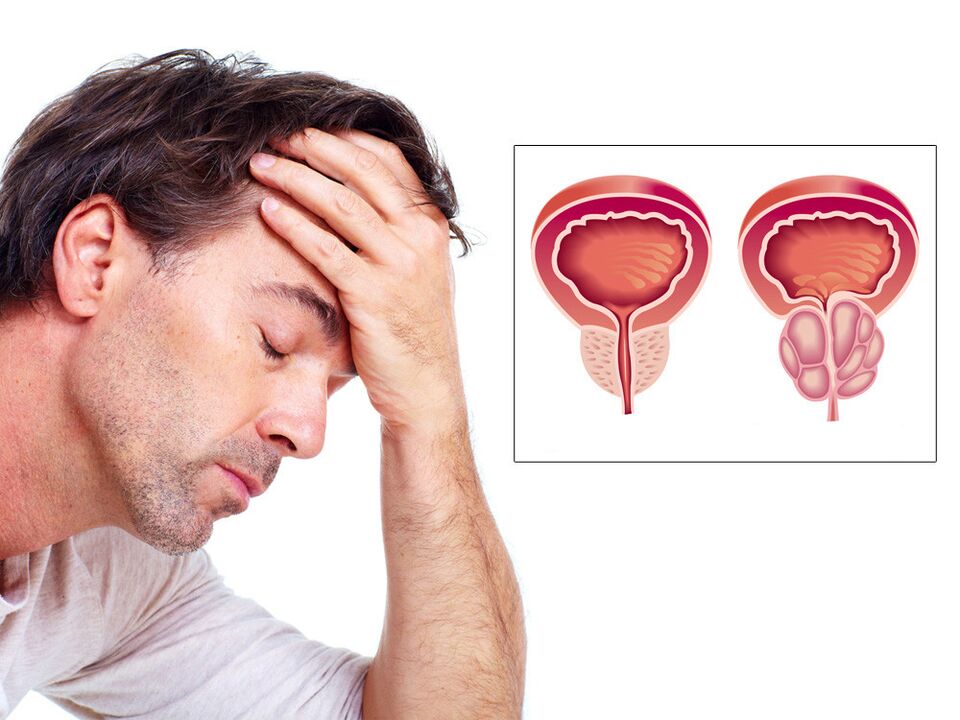
Prostatitis is an inflammation of the prostate gland caused by bacteria. It can be episodic or continuous. This type of prostatitis occurs in approximately one in ten cases. Much more often, men are concerned about another form of prostatitis - chronic abacterial, which is not associated with an infection. Little is known for certain about it, and most urologists do not consider it a true diagnosis. But most problems are associated with it, including problems with sex. Chronic prostatitis is also called chronic pelvic pain syndrome (CPPS).
The pain waxes and wanes
With chronic prostatitis, men are concerned about the following symptoms:
- discomfort or pain in the perineum, lower abdomen, groin, scrotum, penis;
- changes in urination: difficulty urinating, frequent emptying of the bladder in small portions, a feeling of incomplete emptying;
- Some men experience difficulty getting an erection, discomfort during ejaculation, and increased pain after sex. Discomfort can reduce a man's ability to become or stay aroused.
Such problems can occur in men of any age and, according to statistics, affect 10 to 15% of the male population of the United States, most often men between the ages of 30 and 50. Chronic prostatitis cannot be cured with antibiotics, unlike "classic" prostatitis, and its symptoms can bother a man for months or years. They can come and go and vary in severity.
David Lonergan was diagnosed with chronic prostatitis and just three years later found a way to live with it. In the first year, he drank antibiotics, but they did not help (antibiotics do not help with chronic abacterial prostatitis). Here's what David said in an interview with Vice about his feelings:
"At one point I started experiencing wild sensations throughout my pelvic area. At first I had a slight burning sensation in my rectum whenever I sat down. Then the pain became sharp and spread throughout the pelvis. It ended up feeling like hundreds of razor blades were piercing my urethra. On a scale of 1 to 10, I would rate the pain an 11.
Ejaculation became excruciatingly painful. At first I enjoyed the orgasm and relief after it, but hours of pain followed, and when the pain got worse, I stopped having sex. My doctor prescribed prostate massage (the benefits of prostate massage are not proven) and also told me to have sex and ejaculate. But since sex didn't bring any pleasure, I decided to try masturbating once a day. It was a big mistake to do this twice a day - the pain was off the charts (no need to have sex and masturbate through pain, it will not improve your well-being). My wife and I went to a therapist for individual therapy and couples therapy. In many ways, it was she who helped us overcome all our problems in sex.
Most men diagnosed with chronic prostatitis, or CPPS, experience improvement in symptoms within six months. In one study, one-third of men had complete resolution of symptoms after one year. In another large study, one-third of men improved within two years.
Chronic prostatitis is little studied
Chronic prostatitis has not been sufficiently studied. Experts believe there are several potential causes, including autoimmune diseases, genetic predisposition, damage to nerves or muscles near the prostate gland, and hormonal imbalances. Another risk factor can be psychological stress. However, the specific cause can be difficult to determine. Treatment usually involves lifestyle changes and medication to relieve symptoms. Prostatitis cannot be prevented.
Urologist Daria Chernysheva:
- Chronic prostatitis is just a combination of words that can hide pelvic venous congestion syndrome, chronic pelvic pain syndrome, interstitial cystitis, pudendal neuropathy and other conditions. According to the chief urologist of our country, Dmitry Pushkar, this is a stupid diagnosis that the doctor makes to the patient when he does not want to understand what is happening to him. Inflammatory changes in the prostate can be confirmed only with a four-cup test (an analysis in which several portions of urine and prostate secretions are taken). Everything else is overdiagnosis without treatment. To prevent inflammation of the prostate gland, there is a universal recommendation - regular sex life: ejaculation should be at least once every four days, regardless of how it is achieved.
Prostatitis symptoms can be relieved with some simple things, such as a warm bath or heating pad and avoiding alcohol, caffeine and spicy or acidic foods (these can irritate the bladder).
If you have trouble urinating, your doctor may prescribe alpha-blockers - these help relax the bladder neck and the muscle fibers at the junction of the prostate and bladder. Chronic pain is treated with pain relievers. If you have problems with sex, your doctor may refer you to a psychotherapist or sexologist.
Sexual problems are not associated with chronic prostatitis
Urologist Artyom Loktevexpresses the following thoughts: Modern Aspects of Evidence-Based Medicine for Thinking Patients" writes that advertising and the media attribute erectile problems to prostatitis, which is why many men associate them. But this is not true. An erection can be maintained even if the prostate iscompletely removed. According to many reputable urologists, erectile dysfunction in patients with chronic prostatitis is caused by psychological problems. Often, a man's erection decreases immediately after pronouncing the sentence: "You have prostatitis".
Sexologist, psychotherapist, psychiatrist Dmitry OrlovI am also sure that chronic prostatitis does not affect sex life:
"If something happens to the prostate gland, it can affect urination and sensation in the perineal area, but that has nothing to do with sex. Unfortunately, many men and some urologists subscribe to the concept that prostate problems can affect sex life because the prostate is located near the genitals. The prostate gland has a specific function: it produces fluid - a component of sperm. She is not involved in anything else. "
According to Dmitry Orlov, in world practice, doctors almost never make a diagnosis of "chronic prostatitis". It is rather a territorial diagnosis that has no pathophysiological basis, but only a theoretical concept, based on which a person is prescribed treatment. A person hears the diagnosis and startsto worry that this may affect his sexual function. During intimacy, he does not enjoy the process, but monitors how good his erection is. Focusing on the erection can reduce its quality and make the man see a connection between the diagnosisand the problems that arose But the reason is purely emotional.
If there is pain and discomfort during sex, you need to find out the reason for this. It is better to consult a urologist who adheres to an evidence-based approach to medicine.
Dmitry Orlov adds: "If the doctor advises to have sex more often or not to have sex at all, then there must be a medical reason for this. I do not know of any disease in which increasing the amount of sex has resulted in recovery. Most often, such a recommendation is due to the fact that the specialist does not know how to help. It is also not necessary to limit or completely eliminate sex and masturbation, since regular sexual release is beneficial for both the health of the prostate gland and the psyche.
The path from the urologist's office to the sexologist's office is the standard path for men over 35-40 years old. If a man has difficulty with an erection or other problems in sex, he first goes to a urologist, because he considers this to be his area of expertise. If the urologist finds nothing or diagnoses "chronic prostatitis", then only the sexologist's office remains. The sexologist has a wide range of techniques that can help the patient: he can recommend elements of sex therapy, he can engage in psychotherapyor to prescribe medication if necessary. Statistically, this is an effective model of work – on average, the problem is resolved within a month. "






























